A research project headed by a south London university professor has been awarded funding to develop a long Covid rehabilitation programme.
The LISTEN project will work with people living with or recovered from long Covid to co-design a self-management program for people with ongoing symptoms, providing them with necessary support and resources to aid their recovery.
The National Institute for Health Research (NIHR) has awarded £19.6 million to 15 research projects across the UK.
The projects all focus on improving our general understanding of long Covid, from diagnosis and treatment to rehabilitation and recovery.
Heading the LISTEN project is Dr Fiona Jones, 59, a professor of rehabilitation research based in St George’s Hospital and Kingston University, London.
Dr Jones also runs Bridges, a social enterprise program that aids the rehabilitation of people who live with acute and long-term conditions.
She said: “The overwhelming thing that I’ve heard from people is they felt very alone and unsupported, so we hope the resource will be very helpful.
“There’s going to be a clinical trial in 24 different areas across England and Wales, where people with long Covid will be offered one-to-one coaching support by people that have been trained and access to these resources.
“Then we’re going to measure the impact of that on how people get on with their everyday life.”
Dr Jones said whilst there are attempts to define long Covid as having symptoms beyond 12 weeks, it is still a grey area.
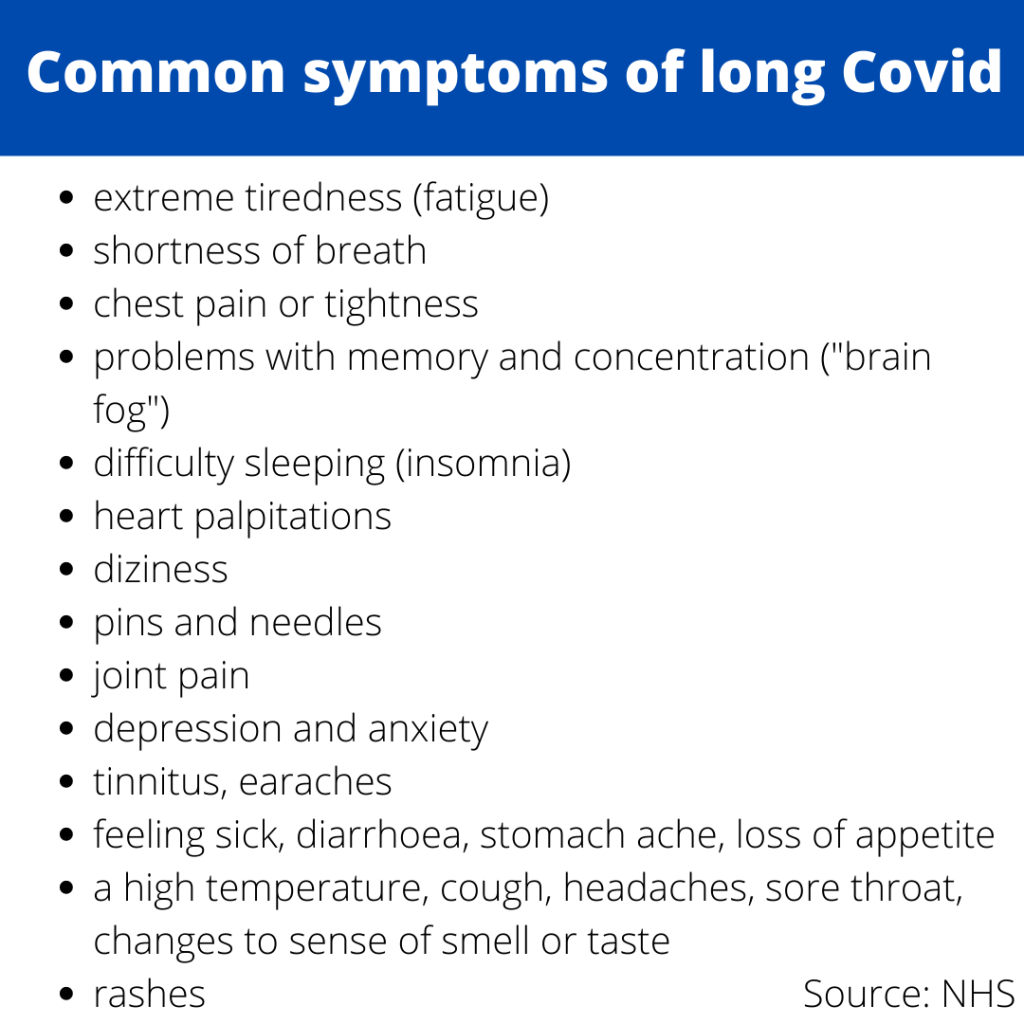
With over 200 different symptoms reported, research like this is critical in order to assist people suffering from the condition.
She added: “Long Covid is a condition which is similar to other conditions where people feel like they’re not listened to by healthcare professionals, or the symptoms that they’re experiencing can’t be explained by standard investigations and so then what happens is they get referred to different departments.
“There isn’t this ongoing support, so there’s not only the experiences you’re feeling, but the anxiety that you’re not getting the support that you need as well.”
Dr Jones stressed the importance of contacting healthcare professionals if you’re suffering with any long Covid symptoms.
“The more that you contact them and tell people about your symptoms, the more awareness they’re going to have to have about this condition.”
Current long Covid statistics and services
Data from the Office for National Stastics (ONS) says an estimated 945,000 people in the UK were experiencing self-reported long Covid on 4 July 2021.
This is down slightly from 962,000 on 6 June 2021.
835,000 people with self-reported long Covid first had (or thought they had) the virus at least 12 weeks previously, and this was at least one year previously for 380,000 people.
A REACT-2 report from Imperial College London found that over 2 million people in England are estimated to have one or more Covid-19 symptoms at least 12 weeks after falling ill.
Dr Jones said: “We’re starting to get data as to who is experiencing symptoms of long Covid and it is in the younger age groups (35-60s) and it’s more women.
“But it also affects people from more socially disadvantaged groups to a higher degree and it effects people who are already living with other conditions as well.”
NHS England spent £34 million on opening 83 clinics for those suffering with long Covid to be referred to.
Private clinics, such as Parkside Private Hospital, Wimbledon, have launched new post-Covid services.
Dr Fhorkan Uddin, 45, a GP at Parkside, explained how they screen patients for long Covid.
“It starts off with the GP services initially because we assess the patient, see what symptoms are predominant, but also we need to screen them for any other illnesses – there are lots of other illnesses that could mimic long Covid.
“We send them for CCG monitoring and sometimes that doesnt bring back anything significant which is reassuring on one hand but doesn’t always explain the patient’s symptoms.”
Patients can also be referred to specialist services, such as physiotherapy or smell training servcies, if they have very specific symptoms.
Dr Uddin gave an insight into the main symptoms of patients experiencing long Covid.
“The first one is general lethargy and feeling tired all the time, the second is shortness of breath – at least 50% of patients that are presented to me have difficulty breathing.
“The third one I’ve seen are issues with smell and the fourth one is palpitations, which is a hard one to quantify.
“If a patient’s having respiratory problems I wouldn’t recommend waiting 12 weeks, I would say come sooner.
“Especially if a patient is symptomatic and it’s affecting their ability to do everyday activities we ask them to come in.”
The realities of living with long Covid
Sophie Bales, 27, had her first dose of the vaccine on June 9 and tested positive for Covid-19 on June 14.
Bales talked about the stages of her diagnoses, the treatment she has received so far and the debilitating effect long Covid has on her everyday life.
“I struggle with headaches, altered sense of taste and smell, a cough, breathlessness, chest pain and tightness, heart palpitations, dizziness, joint aches and pains and extreme fatigue.
“These were all symptoms that were present during the acute phase of Covid.
“The only change is that during the acute phase I lost my sense of taste and smell completely, it has started to come back very slightly over the past week which is over five weeks since testing positive.”
Bales’ concern grew after her symptoms persisted after 2 weeks.
Having being monitored at home under a virtual Covid ward she went back to her GP who suggested her symptoms were most likely due to long Covid.
“My symptoms have hugely affected my daily life – I spend most days at home resting as I am too tired to leave the house.
“If I do have to leave the house I limit myself to one activity a day even if that is just to attend a medical appointment so my week has to be carefully planned to avoid doing too much.
“I am unable to do an activity that requires mental energy for very long as I become too tired.
“I used to be able to go on long walks and swim in the sea, but I am lucky if I can walk for ten minutes without becoming exhausted and out of breath now.
“Being unable to do my usual activities has impacted my mental health making me feel quite low and isolated.”
Bales described her treatment so far as frustrating, as she has to wait a further 6 weeks until she can be reffered to a NHS long Covid clinic.
After being told she may have developed asthma as a result of these symptoms and a potential heart problem, Bales has been told to self-manage her symptoms until then.
She said: “When the symptoms affect so much of your day to day life this is hard to hear.
“The uncertainty and not knowing how long I am going to feel unwell for is also hard to deal with.
“It is difficult to plan anything as I don’t know how I am going to feel on the day so I miss out on seeing family and friends.
“I have seen and had some comments made about some people believing long Covid is psychological and not a physical problem.
“These sort of comments are upsetting when you have to experience the symptoms every day and I wish people could experience long Covid just for a day and maybe they would reconsider their comments, it is very much a real and debilitating illness.”
If you’re reading this and think you are experiencing long Covid symptoms you can express your interest in the LISTEN project by emailing [email protected], or direct message Dr Jones on Twitter at @JonesFIO.




