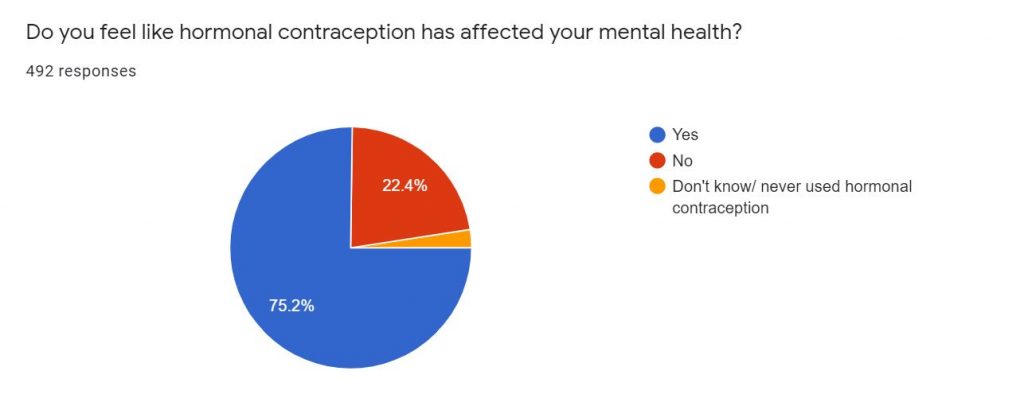
More than 75 per cent of people say hormonal contraception has affected their mental health, shows research by South West Londoner.
It follows a paper published in the Journal of the American Medical Association (JAMA) Psychiatry, that says women who are on the pill are more likely to be treated for depression.
But sadly, experts think an overall lack of research, stigma and the belief birth control is a ‘women’s issue’ could mean doctors are prescribing the powerful hormones – but without fully understanding their side-effects.
Gynecologist Dr Sarah Welsh of HANX believes, ultimately, there is simply not enough research done into hormonal contraceptives, describing some potential effects of the meds as ‘scary’.
She said: “We’re kind of half aware of the fact that they can affect mood, but no one really discusses that.
“A lot of progesterones can induce depression, particularly in vulnerable people.”
She added: “It varies from person to person. We’re all very unique and respond to hormones in different ways.
“Ultimately, the problem is we don’t have enough research on it, and a lot of the studies in medications tend to be done in men.
“Basically, it’s inconclusive in terms of research. But more and more evidence is coming out that there are these side effects that we weren’t aware of. And it’s scary. “
However, in some cases – for instance for people with acne, PCOS or migraines, the pill is a miracle worker.
The women we spoke to told us about their experiences with hormonal contraception, and how it affected their well being.
The responses were fascinating – from feeling like you’re waking up and seeing in colour for the first time, or feeling like your body hates you and the pill is your only saviour.
Here is what they had to say.
Christina Smith, 46, analyst

Christina suffers from what are known as ‘hormonal migraines’, splitting headaches thought to be triggered by the menstrual cycle.
She said during her twenties they got worse, to a point where she would suffer the debilitating headaches sometimes twice a month, for weeks at a time.
She found when she was on the combined pill, a birth control with considerably lower progesterone, she still suffered from migraines.
Christina adds that at the time she was also suffering with an eating disorder and with depression, but found once she switched contraception to the Depo-Provera (medroxyprogesterone acetate) pill, the migraines disappeared completely.
She said: “It was liberating because I didn’t have mood swings. I didn’t have migraines. I didn’t suffer from anything to do with the cycle.”
The 46-year-old consultant enjoyed the lifestyle so much she remained on the pill for ten years, during which time she didn’t have one period.
However, after so long without a menstrual cycle a doctor suggested Christina should get tested for osteoporosis – which some scientists fear could be linked to prolonged use of hormonal contraceptives.
Christina thinks the diagnosis was “definitely as a direct result of being on the pill for so long,” but adds that she was “skinny” too, which could have had a long-term effect on her health.
Since coming off contraception Christina has found her migraines returning, adding the pain makes it feel like her “head explodes.”
Christina said: “I get days where I can’t control my mood and have no sex drive too. So I feel like I’m losing at least two weeks a month.”
She said the migraines coupled with her period and symptoms make it feel like her body hated her.
Ellie Harriss, 23, actor

Ellie said she was first prescribed the pill at age 15, and was on it for around four years.
But after breaking up with her long-term boyfriend, she decided to come off hormonal contraception.
She said: “As soon as I came off it I was a completely different person.
“I was seeing things more clearly, feeling things way more deeply.
“And these were my teenage years – my friends were feeling these really high emotions, even having really high sex drives. And I didn’t have that at all.
“I feel like I went through puberty at 20 because of that.”
However, after entering into a sexual relationship at university, Ellie began to feel condoms were unreliable after a number of ‘scares’.
Ellie pushed for a different type of pill after her previous experience, but it didn’t help.
She said: “I was on it for probably three or four months, and I just felt myself sinking.
“I felt myself going straight back into that whole thing of feeling nothing and really, really low sex drive and low self esteem. I got quite a lot more anxious than I was before.”
Again, Ellie came off the pill and the side effects disappeared. But she still felt like she wanted that extra protection from the pill, so she visited a GP.
By chance this time the doctor specialised in long-term contraception and helped to talk Ellie through all the possible side effects and impact on her mental well-being. That was something she says she hadn’t experienced before.
They settled on the hormonal coil, which Ellie describes as ‘completely fine’.
She added: “I don’t know if that helps things, knowing what to expect, whereas before it was just like here’s a pill packet, go wild.”
Selena Vanamerongen, 20, student

When she was on the pill Selena suffered with hormonal migraines that were so bad they left her vomiting and missing school.
But she found parents and teachers didn’t believe her and even her doctor struggled to make the connection. Eventually they put two-and-two together and realised Selena was one step away from becoming seriously ill.
Selena said her doctor measured her compatibility for migraines and the type of birth control she had been prescribed, finding the then 16-year-old was a three on the chart – which went up to four.
She was then offered a hormonal IUD, and Selena found she was suffering from the migraines less.
However, Selena said it made her acne ‘terrible’.
She said: “It was cystic acne, all over my arms and chest, and it didn’t clear up until maybe the second year that I had the IUD.”
“But by the end of the three years I was doing great on it, I loved it.”
However when it came to replacing the IUD, coronavirus complications saw Selena’s appointments pushed back and she was forced to switch to a different type after her doctor discovered the one she had been on for the past three years was discontinued.
Selena said: “I can say that for my mental health, right now it is not necessarily the best.”
She added that she can’t be sure it’s solely down to the contraception as her mental wellbeing fluctuates with other elements of her life, like her migraines and acne.
Selena said that when she went to get a new IUD fitted her doctor again neglected to discuss any of the potential side effects.
She explained: “She’s like, ‘Do you want another one? Cool. There you go’.”
Natalia Komis, 32, business mentor

Natalia said when she decided to come off the pill no doctors she spoke to were particularly ‘willing or supportive’ to help figure out what was causing life-changing side-effects.
But after years of painful sex and other medical issues, including bumps in her glands and hair loss, she decided it was time to change something.
Natalia said: “I was getting nowhere with doctors.
“This was going on for about five years, and I thought I’m gonna start by stopping putting chemicals in my body and see what happens.”
She added: “I was just not feeling a lot of the time, and not really feeling myself.
“It wasn’t until I came off the pill that things changed and it took a couple of months for me to really realise the difference.
“And now I’m me again, I can feel and see in colour more. I’m the person I remember me being.”
Natalia said when she was on the Serazette pill – which she estimates was for around five years – she had no periods and she remembers feeling ‘masculine’.
During that time she struggled to connect with her feelings and felt she was uncaring and that she barely cried.
At one point, Natalia even contacted her GP, wondering if she could be depressed – but when she suggested it was down to the pill her doctor felt it wasn’t worth discussing.
Since coming off the pill, the numb feelings have thawed.
She found herself reaching for more feminine outfit choices, and reconnecting with her feelings – an emotion she describes as being ‘more Mother Nature’.
Natalia said: “Basically since coming off the pill my sex life has completely improved, and I now have zero problems.
“Obviously that’s down to different reasons, but coming off the pill was 100% part of that.”
Natasha, 29, registered nurse

After getting her first period at 12, Natasha’s cycle was a constant source of stress.
She said as well as an irregular, 37-day cycle she also had issues with weight and excess hair – at which point she was diagnosed with PCOS.
She explained: “At the time my periods were incredibly difficult. For the whole week I just wanted to stay in bed. The cramping was terrible and I was taking a lot of pain meds not even knowing if they helped.”
Natasha says she was desperate for a solution after almost ten years of horrific periods and various medications which seemed to do nothing.
Eventually a doctor suggested the pill, after which Natasha moved onto the implant so she didn’t have to take the pill every day.
Natasha said: “Long story short having contraception has vastly improved my quality of life. I’m worried what will happen when I want to come off it and try to get pregnant but that won’t be for a couple of years.
“I had a lot of chemical imbalances at the time but contraception definitely gave me much more stability mentally.
“It changed a huge part of my life for the better, and that’s not a small thing.”
Dr Sarah Welsh
Dr Welsh says women need to be informed in order to make an empowered decision about their bodies and the type of contraception they choose.
“Doctors should explain to young girls and women that actually there are side effects.
“We should explain what we know around the pill, how it works, and what it does, because you know that then you help them to make the choice that’s right for them.
“Young women need to be educated; making an informed decision is empowering.”
She urged users of hormonal contraception to remember the chemicals they’re putting into their bodies are synthetic, and the release of these into the bloodstream will have an effect.
She added: “So many different kind of chemicals in our brains can change our perception of things, and change how we feel.”
Dr Welsh said more conversation is needed to avoid a contraceptive ‘lottery’, which sees people wasting years of their life trying to find the right birth control.
She added: “Hormones have a significant impact on areas of the brain. And this includes our emotions and our cognitive functions.
“We just need to be conscious and aware that it’s not right for everyone.”




