Contraception usage is falling and rates of sexually transmitted infections (STIs) are increasing at the same time, NHS data has revealed.
In the last 10 years, rates of short-term user dependent contraceptives and long-acting reversible contraceptives (LARC) have reduced by 61% and 19% respectively, NHS Digital Sexual and Reproductive Health Services study data from late September shows.
The rate of people taking oral contraceptives have decreased by two-thirds in the last 10 years, while the implant, the most efficacious contraception with over 99% effectiveness, has decreased by more than a quarter.
Contraception is used for many reasons, mainly to prevent pregnancy but it also can help women with PMS, PMDD and period pain.
Doctor Naomi Sutton, from Channel 4’s TV show The Sex Clinic, stressed the importance of contraception.
She said: “People love having sex, people will always want to have sex and so it’s about how can we make this as safe and as risk-free as possible.
“With contraception we want to stop unwanted pregnancies and allow women to have the type of sex they want to have, which is free of risk of pregnancy.”
Why are contraceptive rates falling?
Naomi says contraceptive rates are falling because of two reasons- lack of capacity in the NHS and social media.
Naomi explained that NHS Sexual Health Services are funded by councils and are generally underfunded and understaffed. Less consultations are taking place, so less contraception can be provided.
GPs’ capacity is also low, and so they are less likely to fit LARC as it takes time.
Moreover, with less help available through doctors, it seems that people are turning to social media to educate themselves about contraception.
Naomi explained that certain sides of social media sell a life with no contraception as happy and worry free, as they often emphasise a hatred of hormone related options and claim contraception can cause cancer and health issues.
Sites like the Lowdown faciliate this, giving women the opportunity to express their opinions about their contraception and since often users only report negative experiences, less attention is paid to good stories.
Naomi said: “I’m not going to go on a site like that and tell everyone how wonderful my Mirena coil is, it’s boring and nobody ever wants to hear dull stories of success.
“People who have a bad story to tell, they will go on it. So I think it’s incredibly skewed towards bad news.”
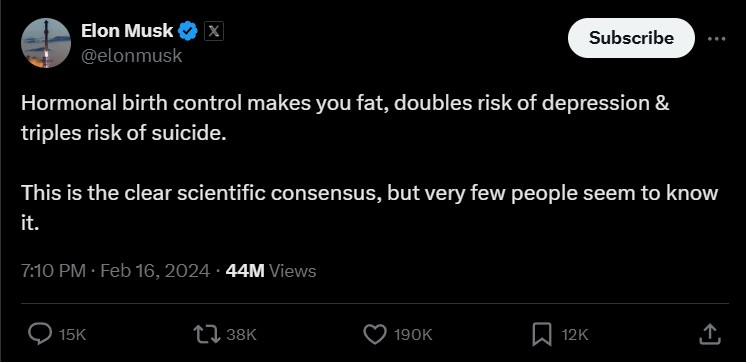
When looking at social media specifically, it is often people with no medical background stirring these feelings, like Elon Musk.
Users like these promote natural methods like natural family planning and the pull-out method over hormonal alternatives.
While contraception can cause side effects at low level rates, Naomi reiterates it is better than the alternative.
She said: “The issue with social media is that they sell it to you as roses and look how healthy and happy I am and they don’t look at the flip side.
“What if you get pregnant? Then what do you do?”
Chloe, an English student from Hampshire said she has seen evidence of this line of thinking on social media.
She said: “I see lots of Instagram posts being like, you don’t need any contraception, it just depends when you have sex on your cycle.
“I would just be too paranoid, I can’t trust that, I trust science.”
Chloe would always use contraception to prevent pregnancy, despite having numerous issues with the pill and the implant, causing her to throw up and have irregular bleeding.
She said: “I really don’t want to get pregnant. If I didn’t have my implant, I would be very paranoid. This provides me with a good sense of comfort that I don’t have to worry about that.”
Louise, a university student from Surrey, also felt like natural methods weren’t for her, despite her implant going too deep in her arm and having to have surgery to remove it.
She said: “I’d rather have the safety net of unnatural methods than just relying on natural methods because obviously different things happen with your body.
“If you’re ill or something, it can throw everything off and then you don’t know what’s where.”
While natural family planning can be used successfully, Naomi said people need to understand that one in four women using this method will get pregnant within 12 months.
Naomi said: “Numbers of terminations are going up, we are definitely using less contraception.”
She explained that if you’re using contraception to not get pregnant, it is better to start with the most effective methods and then work your way down, not the other way round.
This means starting with the implant, then the coil, then the injection, pills, condoms and finally natural family planning.
She said: “It’s about having that tailored discussion with somebody, but this takes skill, and you can’t do that on social media because everybody’s different, and everybody will need that individualized discussion.
“And what frustrates me is that there’s no time.
“GPs don’t have the time, they don’t have the training, they don’t have the education, we don’t have the capacity.”
Condom usage and STIs
NHS Digital Sexual and Reproductive Health Services also reveals the truth about modern day condom usage.
Females making contact with NHS Sexual Health Services for condoms have halved in the last 10 years, while males making contact for condoms have dropped to below a fifth.
Naomi backed this up, and added: “People generally don’t like condoms.”
Diminishing condom use is one of the reasons STIs are increasing.
It is also easier to find sex now more than ever, due to dating apps and online dating.
Naomi explained that we are swapping partners more, but the frequency of sex is going down.
Swapping partners makes contract tracing more difficult, which means it’s harder to tell people they have been injected and if they are unaware, they can spread it to others more easily.
According to UK Health Security Agency data chlamydia has decreased 7%, however Naomi explains this is not the case.
She said: “Chlamydia has always been high, it’s always been our most popular STI.
“I don’t think chlamydia’s gone anywhere and I don’t think we’re winning the war on chlamydia.”
Chlamydia is spread very easily, if you’ve had it once, it’s easier to catch again.
Fourth year medical student Holly said: “A risk factor for getting chlamydia again is if you’ve already had it, the chances of having it again are really really high.”
While the numbers look marginally smaller, this is due to lack of testing.
During Covid there was a lack of testing of all STIs and a lack of funding of sexual health services and less capacity means less testing is still taking place.
Awareness of STIs is also an issue when it comes to tracing.
Holly explained: “A lot of people are asymptomatic to STIs and that can cause a lot of problems because they’re going round not know they’re infected.”
Naomi said that as all STIs can be present without symptoms and screening is key to keeping things under control.
While online testing didn’t exist before Covid, now it has been implemented it does seem to be slowly increasing the methods of testing.
Louise, a student from Surrey, explained that dating around after she came out of a long-term relationship meant that STIs suddenly became a concern for her.
She said: “The testing options are there and they’re free and they’re quite readily available, I got a test within 48 hours the other day and that was absolutely fine.”
Two of the infections which test kits test for are gonorrhoea and syphilis, both of which have more than doubled in the last 10 years.
Since 2014, gonorrhoea has increased by 129%, with syphilis increasing 114%.
Naomi said: “Syphilis is not going anywhere and gonorrhoea is a worry because it’s become resistant to every antibiotic we’ve thrown at it.”
If left untreated syphilis can cause long term complications, including heart failure and dementia, while gonorrhoea is increasingly needing higher levels of antibiotics to get rid of it.
One reason these STIs are increasing is due to the attitude towards them in gay communities.
Naomi explained that for a long time, HIV was a huge worry for men who have sex with men, but the introduction of PrEP and the U=U campaign made HIV less of a concern.
People with HIV who take PrEP treatment can’t pass the infection on to partners, however this means that they are less likely to use condoms as anything else they could catch, like gonorrhoea or syphilis, can be treated.
There were more than three times as many gonorrhoea diagnoses in men than in women in 2023 and more than eight times as many syphillis diagnoses.
Holly said: “Even though we know gonorrhoea and chlamydia are the highest STIs, our teaching has a real focus on men who have sex with men as this is a concern.”
Men who have sex with men may also choose to have sex with women, which also means that the likelihood for women getting these STIs is increasing too, Naomi explained.
STIs are increasing for both sexes and levels of contraception are going down, but not all hope is lost.
Naomi said: “In the UK we are very lucky, we do still have capacity and suitable people but it’s about the general public appreciating the opportunities that contraception provides.
“It is a bit depressing, we need more investment into the right services and better education.
“Education is everything, because you can still find the right service if you know what you’re doing.”
To protect yourself from pregnancy or infection, condom use is advised. For more information on contraception of STIs, see the NHS website.





