Over two million people in England are estimated to have one or more Covid-19 symptoms at least 12 weeks after falling ill according to a new study from Imperial College London.
The government-funded research found that the risk of developing long Covid increases with age, and is more prevalent in women, people who are overweight, smokers, people who live in deprived areas, and those who had been admitted to hospital.
The REACT-2 report from Imperial College London showed that over a third of those surveyed reported persistent symptoms lasting at least 12 weeks.
Around a tenth of those with symptoms said they lasted at least 12 weeks and were severe.
The report found that the risk of developing long Covid increases with age, with a 3.5% increase in likelihood in each decade of life.
North west London-based Jasmin Harsono, 40, developed long Covid after she and her husband caught the virus in mid-December.
Her husband recovered after two and a half weeks, but from mid-January, Jasmin’s long Covid symptoms started to appear and they have continued to get worse since.
She said: “I didn’t have this when I had Covid, but afterwards I started to get this wheezing and chest pain that’s just been continuous.
“Every morning I have coughing for the first hour after waking up and then it kind of dies down.”
Jasmin’s other symptoms include fatigue, brain fog, body aches, and depression.
She added: “It’s quite scary, a few nights ago I was up for about two hours with chest pain which is quite severe when it comes on.
“I still don’t know what it means or what it is, but I’ve had it since January, since Covid.
“When it comes on it feels like a heart attack or something. You have to sit up in bed and take deep breaths while it passes.”
The chest pain is mostly on the left side, on her shoulder and down her left arm.
Sometimes it’s a stabbing pain and sometimes the pain spreads throughout the left side of her body, Jasmin explained.
She has been waiting on an ECG, a test that will look at her heart, since January.
Jasmin, who works in wellness, was generally in good health before and had been able to manage her chronic fatigue, endometriosis, thyroid issues, and depression.
However since developing long Covid, the fatigue in particular is the worst she has ever experienced.
She usually feels a large slump in the afternoon, resulting in her working later into the evening.
The mental health impact of long Covid also takes its toll on those with the condition.
“I have had really bad weeks where I’ve felt really low,” she said.
“I definitely felt a change in me. When you’ve got chronic fatigue every day I think that can affect you anyway because you just don’t have that brain power to do the things that you want to do physically, emotionally or mentally.”
Jasmin’s GP has been understanding, but she has had difficulty accessing further treatment for her long Covid symptoms.
A private doctor arranged for her to have a chest x-ray, but she never received the results.
She said: “My GP has tried to help as much as possible but it’s kind of like their hands are tied.”
Jasmin encourages those who are also suffering from long Covid to continue seeking help, and she hopes to see more conversations and research exploring the condition in the future.
A different study released last week by UCL and King’s College London found that up to one in six middle-aged people who had Covid report long Covid symptoms.
Speaking to SW Londoner, Professor of Public Health at Imperial College London Helen Ward said: “I was surprised at how many people reported persistent symptoms – 38% of people who think they’d had COVID reported one or more symptoms lasting 12 weeks or more.
“But we do have to be careful in how we interpret our findings because many of the individual symptoms are very common, things like headache and tiredness, so we need to dig deeper to see how much more common these are in people who have had COVID than people who haven’t.
“Our research has already shown that the chances of having persistent symptoms increase with age, are more common in women and in people living in deprived areas, and also in people who smoke, have other medical conditions and who had more severe COVID-19.
“Our next challenge is to try and understand why.”
Researchers identified two broad groups of people who reported persistent symptoms at 12 weeks.
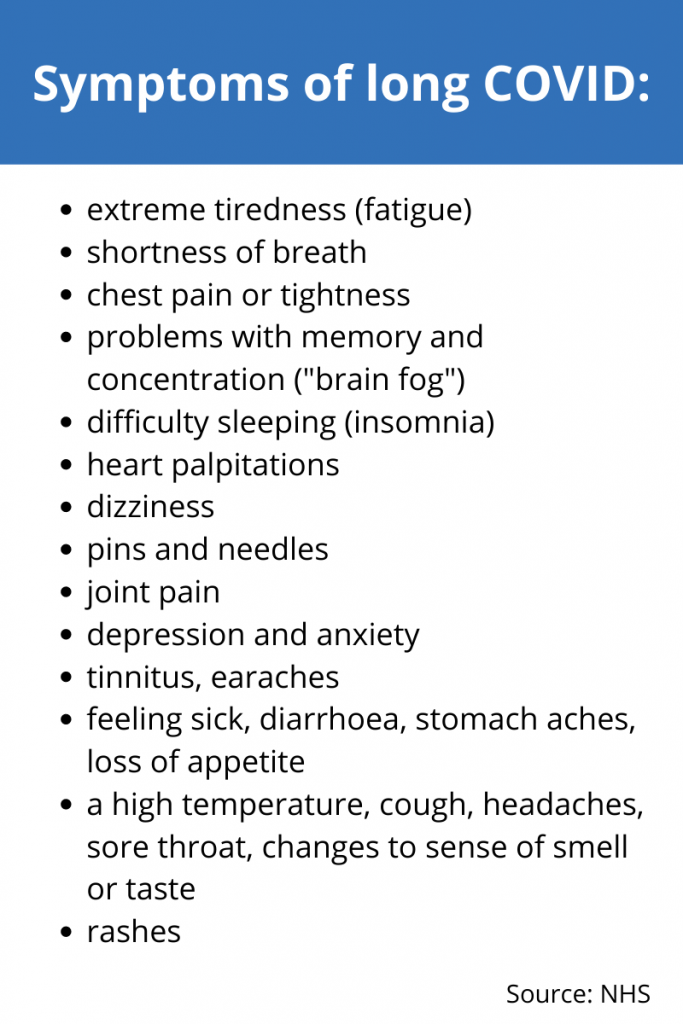
In the first, the common symptoms were tiredness and muscle aches. In the second, the most common symptoms were shortness of breath affecting normal activities, tightness in chest, and chest pain.
Those surveyed were also asked to fill in a free text field where they could indicate other symptoms they experienced.
A number of symptoms, such as “brain fog”, “palpitations” and “hair loss” which were not included in the research questionnaire were reported by those who took part.
Professor Ward said that they are investigating the possible biological pathways of the virus, and they will also measure the role of social and environmental factors.
She explained: “At the moment we don’t know how the natural history of COVID-19 varies with different variants, although there are some suggestions that initial symptoms may be a bit different so that may also translate into differences in long COVID.
“While most people, particularly younger adults and children, will have mild illness if they are infected, some of them will go on to get long COVID and that can be really debilitating. So it is in everyone’s interests to keep the rate of infection as low as possible.
“I would also urge the public, and my medical colleagues, not to dismiss or ignore people with long COVID. They need access to support, investigations and research to develop therapies.”
Professor Ward has also urged people to continue being careful, follow the advice on isolating and testing if you have had symptoms or contact with Covid, and to get both doses of the vaccine when it is offered to you.
For more information, visit the Your Covid Recovery website.




