People who have experienced multiple traumatic events are more than five times more likely to develop Long Covid, a study has found.
The study on medRxiv found that those having experienced two or more traumatic events in the past were 5.6 times more likely to manifest Long Covid, with childhood trauma indicated as potentially escalating the risk.
The European Respiratory Journal found that 42% of patients with acute Covid-19 infection were diagnosed with depression, while 96% had symptoms consistent with PTSD, and their report advocated the use of mental health screening questionnaires in Long Covid recovery.

Dr. Georgina Clifford, Director of London Trauma Specialists, explained: “There is a recognised impact of Covid on cognitive functioning and one of the things I started wondering about is whether there is something about Covid that is impacting the central executive in our brain.
“I have wondered whether Covid is having an impact on that and therefore potentially exacerbating the difficulties people have in regulating their emotions, potentially adding to symptoms of anxiety.”
The similarity in symptoms of PTSD and Long Covid suggests that the two are intrinsically linked.
Dr. Clifford highlighted that PTSD includes symptoms of flashbacks, nightmares, high levels of associated distress, heart racing, sweating, feeling overwhelmed, difficulty concentrating, sleep disturbance, hypervigilance and more.
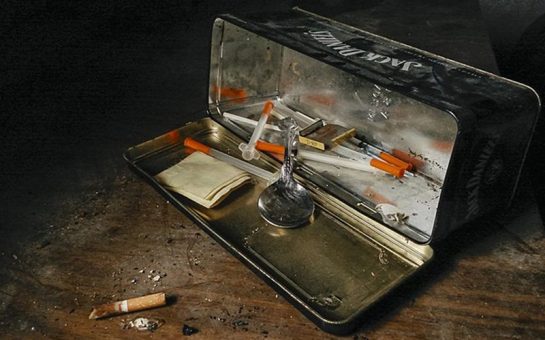
However, with complex PTSD, emotion dysregulation can also develop where people have difficulty managing their emotions, which can lead to people turning to drugs and alcohol, reckless or self-destructive behaviours, and even self-harm.
Additionally, extremely low self-esteem, self-belief and self-worth can develop, making the person feel worthless, hopeless, and like they are broken or damaged in some way.
With Long Covid, recognised symptoms from the NHS include, but are not limited to, problems with your memory and concentration, chest pain or tightness, insomnia, heart palpitations, dizziness, depression and anxiety.
These bare resemblance to the host of symptoms generated in the body by PTSD.

The London Trauma Specialists offer expert insight into how complex PTSD, a form of PTSD developed by a person with a history of trauma such as childhood trauma, affects the brain and body, in a video on their website.
The hippocampus, the filing cabinet of the brain that stores our ‘normal’, organised and accessible memories, allows us to interpret and contextualise our lived experiences.
However, if something happens that makes us feel unsafe, the hippocampus is switched off, and the alarm system, the amygdala, is switched on.
It is this part of the brain that sends the signal to your body that it needs to respond to danger, thus kick-starting the fight or flight response.
As the hippocampus is switched off, the memory of this trauma is not processed in the same way; instead, what is left is a trauma memory.
Trauma memories are inaccessible, giving you little control over them as they can be triggered by environmental reminders at any point, inflaming all the emotions and bodily feelings experienced at the time of the event, convincing your body it is in danger again.

A lot of the time, the brain’s attempts to fit a trauma memory in its memory filing cabinet causes an individual to express avoidance behaviours and strategies to stop or suppress the memory, as it is just too difficult to process.
However, the more the memory is stifled, the more agitated it can become as it is left unprocessed in the brain, making it more volatile.
Those with a history of trauma will have many traumatic memories heightening the body’s fight or flight system, where each time these memories are triggered, the body is convinced it is in danger.
Living in this heightened state of vigilance has massive physical repercussions on the body.
As this data has started to reveal, one of the consequences is that the body’s ability to recover from illness is weakened by the relentless fight or flight response.
Hence, those with a history of trauma, those who appear healthy, active and busy, can be prone to having weaker immune systems and therefore face a higher risk of developing Long Covid.
Dr. Clifford explained how she frequently works with a lot of police officers who, at the end of a career filled with trauma, are faced with symptoms of complex PTSD and huge amounts of physical health conditions as well.
She said: “What you have got is somebody who is experiencing very extreme and quick responses to threat, which is where the hypervigilance and jumpiness comes in, where people live their lives as though they are constantly faced with something threatening, and it takes them longer to get back down to a state where they can feel relaxed again.”
Using police officers as an example of how people with a history of trauma can end up with a host of overwhelming physical symptoms that detriment physical health, Dr. Clifford explained that having a history of trauma could therefore play a hand in increasing the risk of an individual developing Long Covid.
Dr. Clifford emphasised that what a lot of studies show is that most of the young, healthy adults with Long Covid are individuals who previously had very busy, active lives.
This indicates that those with Long Covid are likely to be the kind of people who find it hard to relax, sit still, and in some cases may have a form of high-functioning anxiety.
However, in order to recover from something like Long Covid and PTSD, the body has to be able to completely relax in order for the fight or flight cycle to be broken.
She said: “If you’ve got people who have got Long Covid and a history of trauma, you’re saying actually you need to be able to convalesce, you need to be able to take yourself to bed, you need to be able to stop.
“But if what’s happening is those people who stop then get a flood of all that stuff from the past and they don’t have the adequate mental health support in place to help them with that, then that’s incredibly difficult.
“They are then more inclined to get up and use those strategies that have worked in the past that push it away and block it.”
This implies that for some Long Covid sufferers their mental health could be hindering their recovery.
Acknowledging mental health support in Long Covid recovery is therefore crucial.
The consistent pushing down of difficult emotions, the inability to relax and an extremely busy lifestyle is often an indication of a survival personality, and this is frequently a result of childhood trauma.
Health coach and former osteopath Sorrel Pindar, who has been working with Long Covid patients, consistently notices that patients struggling with long-term illnesses such as chronic fatigue or Long Covid have survival personalities.
She said: “As a child you develop strategies that allow you to survive, but they are not actually terribly functional in adulthood.
“Whatever we did as children, we did it in order to survive.”

Once again, a history of trauma, where people are made to feel like they have to fight to survive, puts them at risk of long-term illness as the immune system is depleted by years of stress-induced systemic trauma.
Sorrel noted: “Everybody I have worked with had a survival personality.
“I would say Long Covid is a physical expression of a psychological trauma.”
Because of this, Sorrel’s approach to helping her patients centres around breaking down their survival anxiety, so that they are able to rest and recover.
In order to recover, Sorrel noted that patients need to be able to trust their body’s ability to recover, because a lack of bodily trust causes sufferers to fixate on symptoms, which simply fuels the trauma on the sympathetic system of the body.
This is often where osteopathy can be extremely beneficial.
It can be deeply calming, Sorrel explained, as the rocking motions and mobilisations evoke the feeling of being back in your mother’s womb or being rocked as a baby, and for anyone, not just those with a history of trauma, this can remind the body to let go of its pent-up anxiety.
Osteopathic treatments offer the opportunity for the body’s fight or flight cycle to be broken, which, if it has been active for a long period of time as is the case with those who have a history of trauma and survival personalities, can be inducing daily physical symptoms on the body.
It has been recognised that those with Long Covid are likely to develop depression and anxiety.
However, it is not just vital that mental health support is provided for Long Covid sufferers.
This data suggests that it is also important that screening is included in Long Covid rehabilitation to determine whether trauma-related suffering and having a survival personality could be implicating the individual’s chances of recovery.
Feature Image: Heike Trautmann, Unsplash